THE NHS WORKFORCE BY NUMBERS

The NHS or National Health Service is a publicly funded healthcare system in the UK which offers essential services to residents. It provides Government-funded healthcare to all UK citizens based on their need for healthcare rather than their ability to pay for it. It plays a major part in employment in England employing 1.5 million people.

This NHS is one of the largest employers globally, hiring workers that cover a vast range of positions, from nurses to technical staff and employs people from a diverse range of backgrounds. It is of a multi-disciplinary nature, relying on health care scientists, physiotherapists and occupational therapists, which demonstrates how important it is.
However, despite its size, figures suggest it doesn’t have enough staff to meet demand. Many factors come into play including the Covid-19 pandemic and the significant impact it has on workloads and working patterns of medical staff.
Here we will take a look at the figures and statistics in relation to the workforce in the NHS and why these figures exist.
What kind of workers make up the NHS?
Professionally qualified clinical staff make up around half of all employees which the NHS is heavily reliant on. Other key staff groups include those working in:
- Central functions.
- Dealing with the NHS’s property and estates.
- Supporting clinical staff.
The vast majority of NHS staff (1.2 million full-time equivalents) work in ‘hospital and community services’ (HCHS) as direct employees of NHS trusts. They provide ambulance, mental health and community and hospital services including 21,000 staff workers that work as local planners and commissioners of health services. Around 150,000 work in primary care which includes general practice, community pharmacies and dentistry.
Across NHS hospital, community and primary care settings, there are:
- 164,000 doctors.
- Around 360,000 nurses and midwives.
These two groups make up just over a third of the total workforce which demonstrates the vastness of the NHS.

The composition of the NHS workforce as of March 2022
The below figures focus on staff directly employed by NHS organisations including general practice.
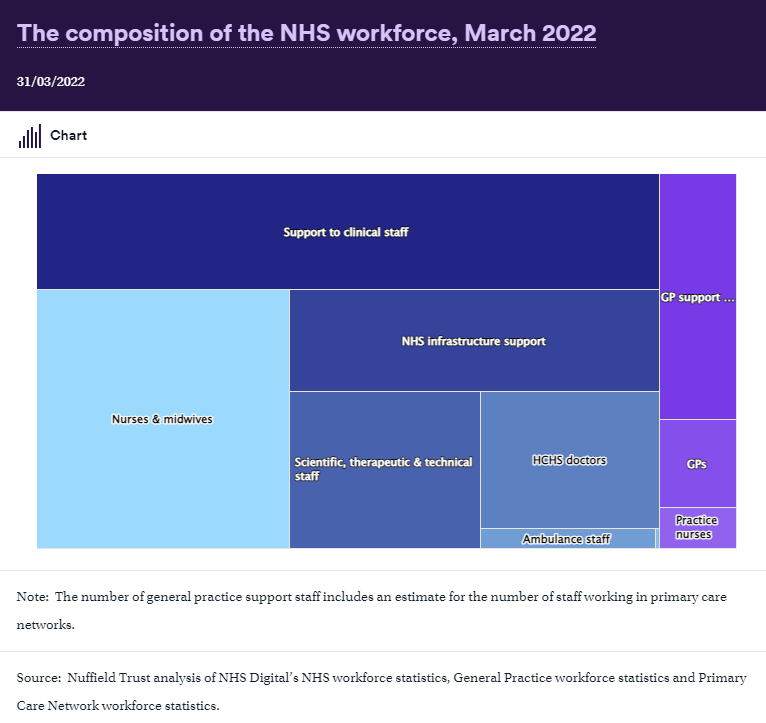
- Nurses and midwives: 343,651
- Ambulance staff: 18,095
- Support to Clinical Staff: 379,133
- GP support and admin staff: 99,359
- NHS infrastructure support: 199,250
- GPs: 35,626
- Scientific, therapeutic and technical staff: 157,706
- Practice nurses: 16,629
- HCHS doctors: 128,392
Diversity within the NHS
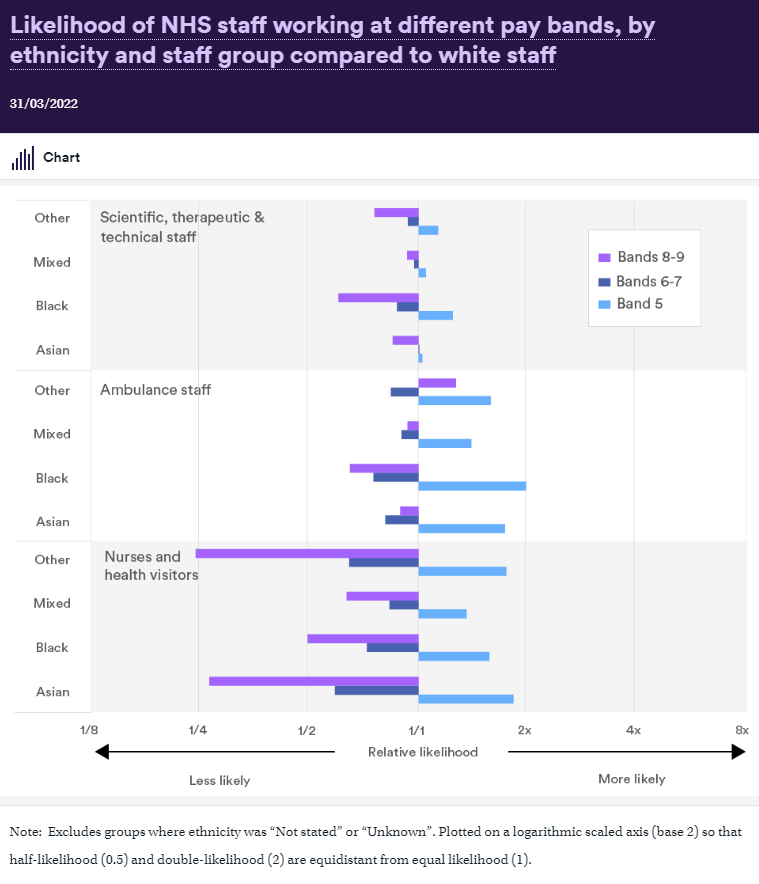
One quarter (25%) of NHS staff are of Asian, black or another minority ethnicity, compared to 13% of all working-age adults in the UK. However, these statistics vary by staff group and staff grade.
Other characteristics to consider are age, gender, disability, religion and sexual orientation to ensure that the NHS workforce is sufficiently diverse and reflects the society it serves.
What kind of shortfalls have occurred within the NHS?

Published data suggests there were 105,855 vacancies (8%) in the NHS between January and March 2022, however, it can be difficult to be completely accurate as some vacancies are filled on a daily basis by temporary staff and other reasons for absences may include sick leave. These shortages are spread out unevenly throughout the country. Of course the Covid-19 pandemic has a major part to play. It has been reported that the number of staff absent from work on one day reportedly reached over 120,000 during peak pandemic times.
Reports suggest the highest percentage of full-time equivalent vacancies was in London (10.9%) and the lowest in the North East and Yorkshire (6.1%) These list of figures are available to view by region here.
Shortages within hospital services

Hospital Doctors
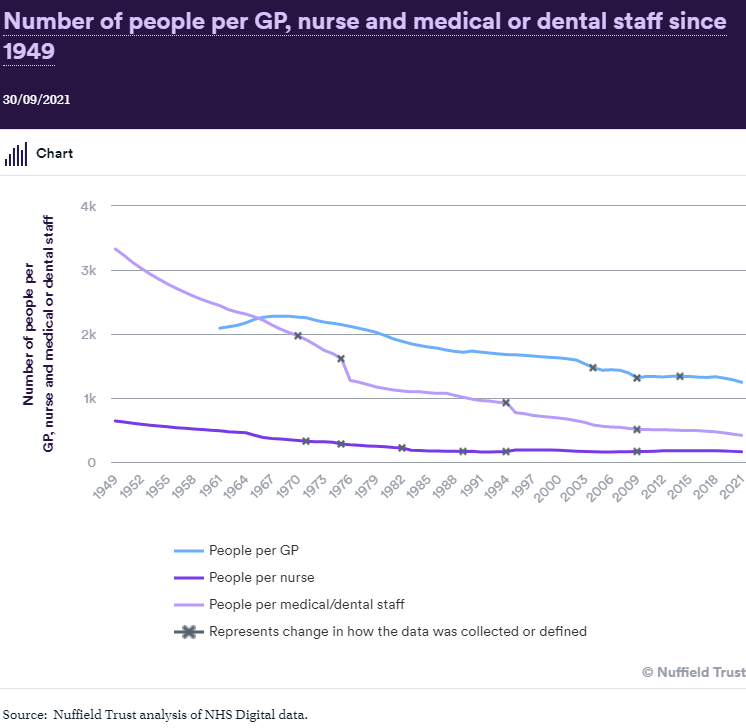
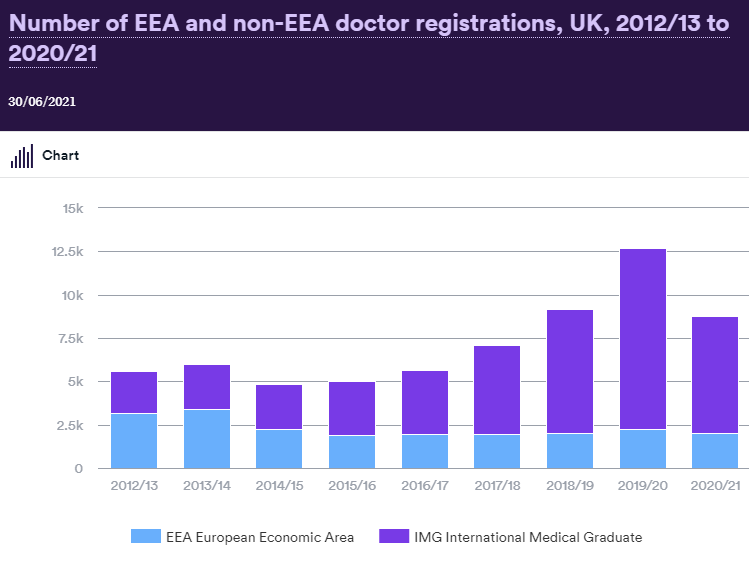
There was a 64% increase in hospital medical staff, growing from 78,000 in September to over 128,000 in March 2022 and the number of hospital consultants has risen by 89% (from 28,000 to 53,000). However, hospitals are still experiencing difficulties with staffing medical professionals across multiple specialties and locations.
Shortages mean there are not enough senior or medical staff to assure the quality and safety of training. This in turn, means junior doctors may be withdrawn from hospitals, further reducing staff. Because of the Covid-19 pandemic there have been a range of staffing issues with one in six doctors reporting that one of the main changes from the pandemic was the change in their rotas.
Nurses
In 2015, nurses were added to the list of shortage occupations by the Migration Advisory Committee (a non-departmental public body that advises the Government on migration issues), this was initially on a temporary basis. However, in October 2019, nursing still featured as a role experiencing significant shortages.
The number of full-time equivalent nurses has fluctuated in recent years but, on average, numbers have increased by less than 1% a year between 2009 and 2020 (from 278,500 to 298,600 in February 2020).
However, since the start of the Covid-19 pandemic until March 2022, the number of nurses substantially increased by over 21,100 (7%).
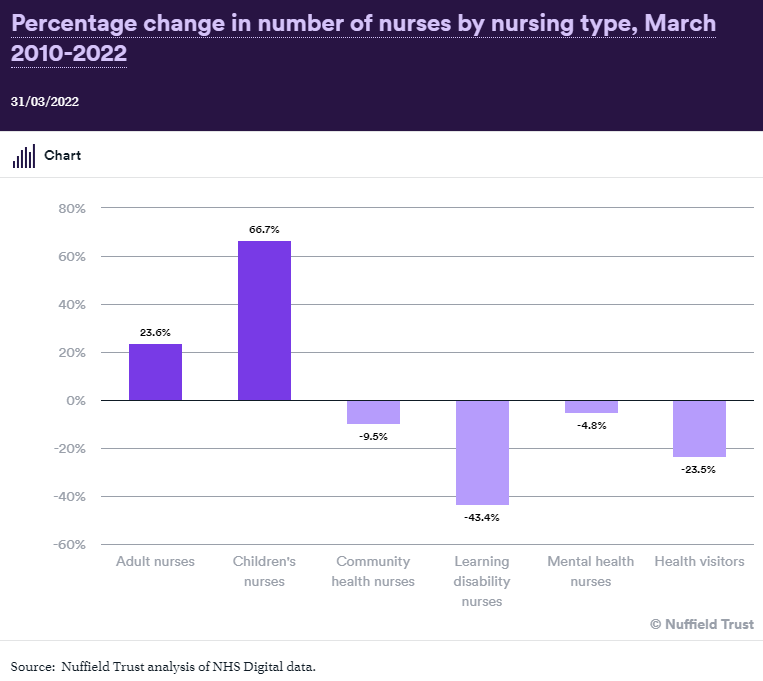
Figures vary depending on specific types of nursing as we can see below.

The number of learning disability nurses fell by 43% (from 5,500 to 3,100) in 12 years from 2010 to March 2022.
The number of children’s nurses increased by two-thirds (67%) for the same period (from 15,100 to 25,100).
You can see the below chart in relation to the percentage change in the number of nurses by nursing type from March 2010-2022.
Mental Health Staff
Around 133,000 people are employed by the English NHS to care for people who need mental health services. The number of registered mental health nurses have been in decline and there was a 5% drop in the number of nursing posts between March 2010 and March 2022. However, there is a lack of clarity in relation to the roles within mental health services which leads to complications when increasing the size of this workforce.
There have been a shortage of psychologists who are a key group within the mental health sector. There is an implementation plan to have an additional 8,130 psychologists and psychotherapists working in mental health by 2023/24. There is also an ambition in the 2019 mental health implementation plan for an additional 26,000 staff to work in mental health services by 2023/24.
Ambulance Staff

Yearly increases saw full-time equivalent ambulance staff numbers rise from 31,000 in March 2010 to 43,100 in March 2022. Paramedics were the main reason for this growth which had a 61% increase since 2010. However, changes in the way data is collected has resulted in difficulties in reporting trends for ambulance support staff. There is still a shortage of ambulance staff with employers competing with one another.
Ambulance staff deal with a number of challenges on a daily basis and score low on matters of equality, diversity and inclusion; health and wellbeing; morale; and working in a safe environment, amongst others, according to the NHS staff survey.
Scientific, Therapeutic and Technical Staff
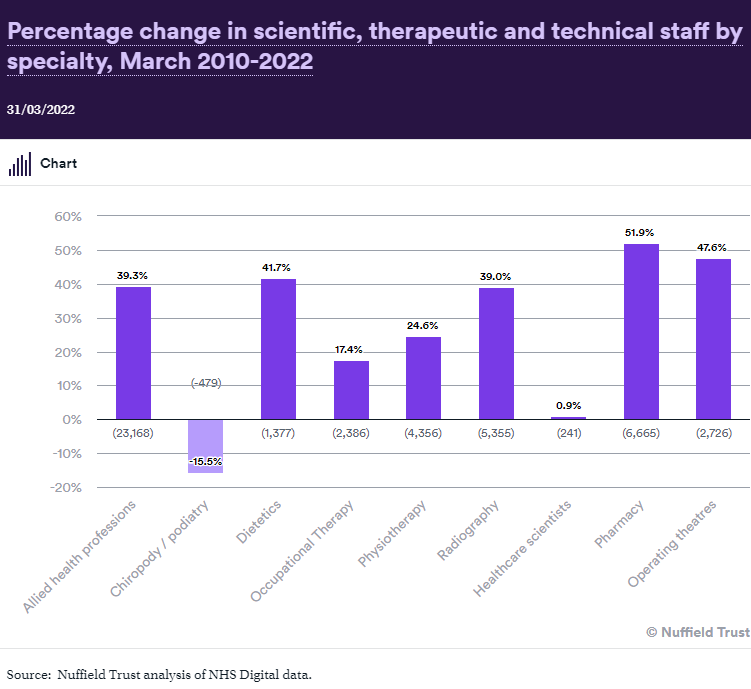
There were over 157,000 ‘scientific, therapeutic and technical’ full-time equivalents of qualified clinical and scientific workforce professionals as of March 2022 and this group has increased by 31% since 2010. While the number of operating theatre staff has increased by 50% and radiography staff by a third, the number of chiropody/podiatry staff has fallen by 12%.
Clinical Support Staff
These consist of frontline staff who are not typically registered professionals, however they deliver a large amount of hands-on patient care. Numbers in this group have risen from 288,000 in 2010 to over 379,000 in 2022 – an increase of 32%.
Shortages for staff delivering care close to patients’ home
Primary Care
There has been no progress against the 2019 target set by the UK government to increase the number of GPs by 6,000 by 2024 even though there was a 2016 ambition to increase the number of GPs to 5,000 by 2020 which didn’t succeed. There has been a decline of 387 fully qualified, permanent GPs working in England since 2019 with deprived areas having fewer GPs per person than less deprived areas.

The number of practice nurses has remained around the 24,000 mark for several years equating to 17,000 full-time posts as seven out of 10 practice nurses work less than full time. Over one-third of these staff (35%) are over 55 years old.
In early 2019, NHS England initially committed to fund 20,000 more staff in primary care, including pharmacists, physiotherapists, paramedics, physician associates and social prescribing link workers, this increased to expanding staff working in general practice by 26,000 by 2023/24.
Community Health Nurses
Since 2009 there have been significant falls in the level of nursing in community health services and health visitor numbers have also dramatically fallen by over one-fifth in the last three years. The figures do vary however depending on different roles in which you will find listed here.
Implications of these shortfalls
Some shortfalls are filled by temporary staff which provides flexibility to the employer and employee, however it can sometimes lead to negative consequences such as:
- Costly to already strained finances.
- Disruptive to health services.
- Reduces the ability to deliver continuity of care to patients.
However not all vacancies are filled. Analysis having suggested that the NHS may have had some 1,400 unfilled doctor vacancies and up to 12,000 unfilled nursing vacancies on a given day. With staff burnout due to Covid-19 pressures and staff vacancies being related, it is clear that a need to tackle these shortages is evident.
Reasons for these shortages
It is evident that the government’s goals have been difficult to achieve, such as 50,000 more nurses over a 5-year period. However, the number of nurses has increased by 10,500 within the last year alone creating optimism.
There have been specific pressures to increase staff in response to safe staffing guidelines and to meet the targets as detailed in key policy documents such as the GP Forward View and the NHS Long Term Plan. A demand on the health service has grown dramatically over the last few decades. Key factors that play a part in the shortfalls are:
- A failure to train sufficient numbers of staff with a high proportion of university students not completing their nursing courses.
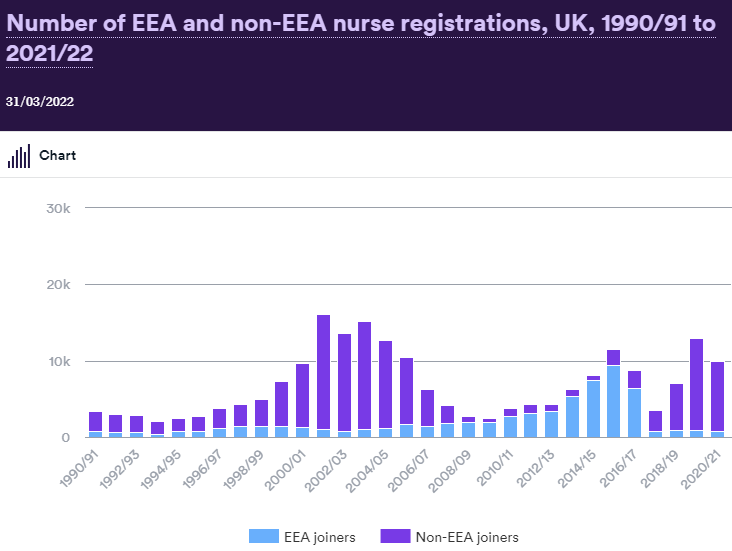
- The health service has a heavy reliance on international recruitment in fact one-in-six (16%) of hospital and community sector staff were recorded as having a non-British nationality as of March 2022 with fluctuations occurring over time. However, recruiting from less developed countries tends to bring up some ethical issues.
- The number of hospital and community health staff leaving the NHS has grown considerably.
- This particular workforce has often been overlooked in previous NHS policies and plans.
As a result of Brexit, nurses who trained in the EU and want to work in the UK are now subject to the same application process as those who trained outside the EU. This has implications, for example, for the fees and the skills and knowledge tests that have to be undertaken for those looking to join the UK nursing register.
How does the UK compare to other countries?
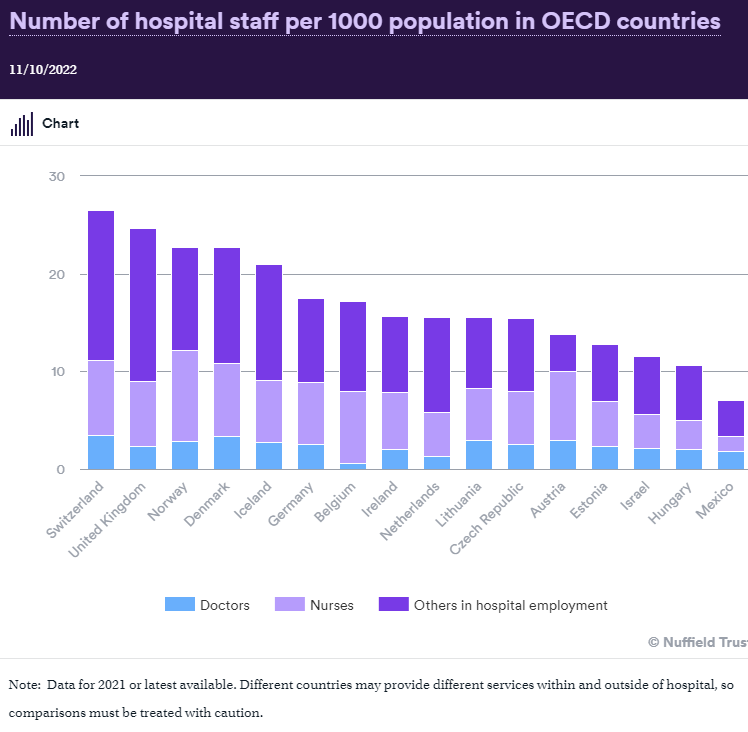
It is difficult to get accurate data when comparing the UK to other countries because of differences in:
- Geographies.
- Service Design.
- Data.
What does the future look like for the NHS?
It is evident that there are serious staff shortages within the NHS which will not be easy to overcome. Clinical professional are leaving and finding replacements is difficult. Age also plays a part, for instance, in the nursing professions there is a large proportion fast approaching pensionable age.
- 27% of nurses are aged between 45 and 54.
- More than one in six (17.6%) are aged 55 and over.
- In midwifery 4 in 10 midwives are already over 45 and eligible to consider retirement at 55.
For the full list of these figures and statistics, you can view them here.
Of course, the government’s response to the Covid-19 pandemic may have influenced a large proportion of the above trends and statistics. It is clear the NHS faces numerous challenges influenced by the political climate as well as economic instabilities and that resolving staffing issues clearly needs to be a priority.
There is plenty more to read up in relation to his topic with all of these figures and statistics available for you here.
Take a look at our previous blogs below:
Protected: Recent Updates To The Employment Permits Act 2024
Recent Updates To The Employment Permits Act 2024 The Employment Permits Act 2024 has introduced several recent updates that came into effect on Monday the 2nd of September 2024, aimed at improving the employment permit system in Ireland to make it more flexible, modern, and responsive to the current needs of the labour market. There are…

How Can I Get a Job as a Nurse in the UK?
How Can I Get a Job as a Nurse in the UK? Becoming a nurse in the UK is a rewarding career choice that not only offers the chance to make a significant impact on patients’ lives but also provides a stable and fulfilling profession. The question how can I get a job as a…

Guidance And Support For Prospective Overseas Candidates
Guidance And Support For Prospective Overseas Candidates NHS Employers is distributing an update from the Department for Health and Social Care. It states that the guidance for international applicants seeking health and social care jobs in the UK has been revised and reissued. This guidance and support for prospective overseas candidates offers assistance by providing…

Nurses and Care Workers Immigration Policy Update
Nurses and Care Workers Immigration Policy Update At Servisource, we strive to keep healthcare workers updated with the latest information. Back in December 2023, the UK government revealed adjustments to the immigration system, and it has been revealed that these adjustments are set to be enacted in March and April 2024. The timeline for implementation…

New Immigration Rules Introduced by the UK Government
New Immigration Rules Introduced by the UK Government On 4 December 2023, new immigration rules were introduced by the UK government. These changes to the immigration system will take effect from Spring 2024. The upcoming changes to the Health and Care Visa route will specifically impact the care sector in the UK. Under these changes,…

How to Support Men’s Health this November
How to Support Men’s Health this November Movember, the global movement that has taken the world by storm, encourages men to grow moustaches during the month of November. This movement raises awareness about how to support men’s health, particularly prostate cancer, testicular cancer, and mental health problems. In the United Kingdom, this movement has gained…
